Exodontia or dental extraction is, undoubtedly, the dental procedure that people report they dread the most. Unfortunately, it’s because we automatically associate it with pain, or the ‘bad dentist’ scene from the “Little Shop of Horrors†movie, directed by Frank Oz! However, sometimes, we are left with no other option but to have a dental extraction, and here is what you need to know…
Dental Extractions Are a Type of Oral Surgery
Although pulling wisdom teeth isn’t a complex procedure, there are some risks and common complications that can follow a procedure. The bottom line is that like any other surgery, certain post-surgical complications could occur. However, there are many variables and factors that could predicate a patient developing complication. First of all, there are different types of extraction surgeries, and risks of complications will vary.
So, while the risks are not usually very serious, it’s better to educate yourself on things that could potentially go wrong. It’s also important to know how you can prevent and/or treat them before your procedure. OMSH provides information below about some of the most common complications that can occur after an extraction:
1. Extensive Swelling, Pain, or Bleeding
Experiencing some swelling, pain, or bleeding after a tooth extraction is completely normal for every patient and will happen for at least a day or two. However, if any of these factors become more severe and do not subside after 24-48 hours, contact your oral surgeon. Your persistent symptoms could possibly be a sign of an infection.
Unusual Swelling
Typically, the swelling goes away or at least starts reducing after a couple of days. But inform your doctor if the swelling persists or increases after 3 days. You will also want to contact the oral surgeon if you are experiencing excruciating pain with swelling.
Persistent Bleeding
Your bleeding should ideally stop within a few hours after a dental extraction. Yet, there are a few factors that could cause persistent bleeding and you should contact the oral surgeon immediately. For example, if you sustained an injury during or after surgery and you need stitches, or if you’re taking anticoagulant medications. Anticoagulant and antiplatelet medications are two common forms of blood thinners that increase the risk of bleeding. So, if you’re on these medications, or taking aspirin, notify the surgeon well in advance of the procedure. The oral surgeon will advise you on when to temporarily stop and restart these medications.
2. Dry Socket
Alveolar Osteitis is the medical term for what we commonly know as a dry socket. Unfortunately, dry socket is one of the most common complications people experience after tooth extractions. When the blood clot forms on the extraction site it could become dislodged prematurely. And as a result, the absent clot will expose your jawbone and nerves to air and food particles.
Dry socket can typically develop two to three days after the procedure when you do not follow post-surgical aftercare instructions. It causes severe pain, which may spread to the ear and throat, and result in an unpleasant taste or odor. At the same time, if you do not seek treatment right away, a dry socket could turn into a serious oral infection.
Who Is At Risk?
Dry socket is more common in cases where dental patients have lower jaw extractions, and for people who are smokers. This is why dental practitioners advise to not smoke for several days after the surgery. Women who take oral contraceptives also have a higher risk of developing a dry socket.
However, the condition most commonly develops due to not following the care instructions given by the dentist. Examples include using straws to drink, eating and chewing directly on the surgical site, and brushing/touching the surgical. All of these actions could put you at a higher risk of developing this complication.
Overall, surgeons will treat dry socket with pain killers and antibiotics. They may also provide medicated dressings to help encourage the development of a new clot.
3. Infection
An infection can develop at the extraction site for various reasons and cause swelling, pain, and high fever. With an infection, you may start to develop flu-like symptoms, fatigue, and feel miserable overall. Also, you may notice a white or yellow discharge from the dental extraction site. Making a diagnosis generally requires an examination and perhaps an x-ray. If you do develop an infection, you’ll need to take antibiotics (most likely for an extended period) for treatment.
4. Nerve Injury
Though extremely rare, nerve injuries during dental extraction surgery could occur. This type of complication usually happens if a dental nerve is in a peculiar place and sustains damage during the procedure. This could result in a tingly feeling or numbness around the gums, tongue, chin, and lower lip.
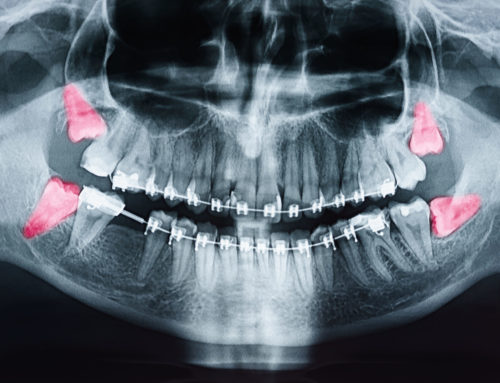
Fortunately, if there is nerve damage, its effects are usually temporary. Experienced oral surgeons commonly avoid this issue by viewing x-rays prior to surgery. This way, they know the location of nerve endings and the best way to remove the tooth without affecting nerves.
Following Dental Extraction Aftercare Instructions
There are a few other complications that you could develop after a dental extraction, like maxillary bone infection or others. However, these kinds of complications are extremely rare and very uncommon. When and if patients develop post-surgical complications, it’s usually because they did not follow aftercare instructions. So, we can prevent the majority of complications simply by strictly following the instructions given by the oral surgeon. Also, it’s important to allow yourself the proper time to heal. So, get your rest.
And, should you have any questions or concerns about a recent dental extraction please call OMSH at  713-804-6055.